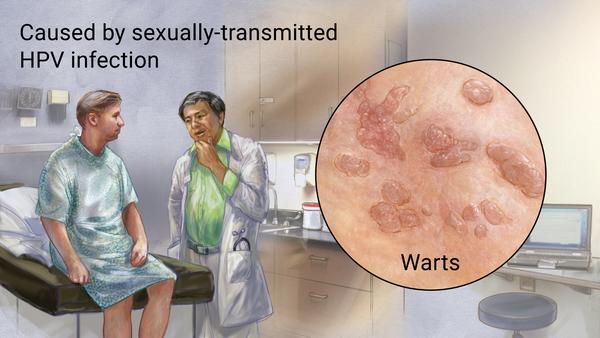
Condyloma acuminata:
Cause: HPV 6,11 while HPV 16, 18 causes Cervical cancer
Symptoms: 90% HPV no symptoms, warts on genitalia & mouth, can spread to other parts by touching/auto-inoculation.
Transmission: Sex: Vaginal, anal, Oral; Childbirth; Sharing clothes; auto-inoculation.
Inv: Pap smear to detect Cervical Dysplasia, Characteristic finding: Koilocytes (Large nucleus surrounded by Halo)
DX: Clinical inspection sufficient.
Biopsy of Wart, DNA Hybridization test (Swab sample).
RX: Observation as most resolves within 1-2 years except Anogenital warts.
Surgical: Burn of the warts using Liquid Nitrogen or Salicyclic acid.
Topical: Podophyllin (Podofilox), Imiquimod, Trichloracetic acid .
Prevention: Condoms, Dental Dams, For Child Birth with Mother HPV – C Section is done.
HPV Vaccine prevents HPV 6,11,16,18, for Penile and Cervical cancer prevention (Recommended for female age 9-26).
Differential Diagnosis:
Condyloma Lata: Manifestation of Secondary Syphilis. Warts tend to be smooth, flat-topped, larger.
Clinical: Look for recent hx of primary chancre (past few mod).
May be accompanied by other signs of secondary syphilis, I.e., constitutional sx (malaise, fever, H/A, nausea), lymphadenopathy.
Dx: RPR/VDRL. Rx: Benzathine Penicillin.
For Cervical Cancer:
Pap Smear:
Woman 21-65 once Every 3 years
Pap smear & HPV Testing:
Woman 30-65 once Every 5 years if HPV is negative.
To get the most accurate results, Pap smear should be taken when one is not menstruating and avoided sexual intercourse, douches, or vaginal suppositories for 48 hours beforehand. This is because these fluids may alter the results of the lab tests.
Case Scenario 1:
A 24 year old man comes to the clinic because of 2 “bumps” on his penis and scrotum. The lesions have been there for approximately 7 months and have been progressively larger. They are not painful. He is sexually active with 2 female partners, who are both on oral contraceptive pills and so they do not use barrier contraception. He had chlamydial urethritis last year. His temperature is 37.0 C (98.6 F). Physical examination shows a 3mm flesh-colored, non-tender, lesion with a “heaped-up” appearance on the shaft of the penis and a 4mm lesion with a similar appearance on his scrotum. The remainder of the examination is unremarkable. A rapid plasma regain (RPR), VDRL, and flourescent treponemal antibody absorption (FTA-ABS) test are all non reactive. In addition to providing the appropriate treatment, he should be told that:
(Note: Since RPR, VDRL, FTA-AB are non reactive, it is not syphilis)
A. Condoms will prevent the spread of this disease to future sexual partners
B. His sexual partners should be evaluated because they may be at an increased risk for cervical cancer
C. Oral suppressive therapy will decrease the frequency of recurrences
D. The state health department will be contacted because this is a notifiable infectious disease
E. Treatment will eradicate the infection
Ans. B
Case Scenario 2:
A 24-year-old woman comes to the clinic for a periodic health maintenance examination. She has no complaints. She exercises daily, eats a low fat diet, drinks “a couple of beers” with friends on the weekends, and is a “social” cigarette smoker. She has multiple sexual partners and uses oral contraceptive pills as birth control. She does not use condoms because “it is not as pleasurable”. Her blood pressure is 110/70 mm Hg and pulse is 60/min. Her physical examination is unremarkable. You perform a pelvic examination and send a Pap smear to the laboratory for evaluation. The results, which return 5 days later, show two superficial squamous cells with sharply demarcated, large perinuclear vacuoles and alterations in the chromatin pattern. They use the term “koilocytic atypia.” At this time the most correct statement about her condition is:
A. Acyclovir will decrease the shedding of the organism
B. Her Pap smear findings are unrelated to her sexual activity
C. She and her sexual partners should be treated with metronidazole
D. She may be at an increased risk for developing cervical cancer
Ans: D.
Case Scenario 3:
A 37-year-old man comes to the clinic because of bright red blood on the toilet paper with bowel movements. He can also feel “bumps” around his anus and wonders if they are hemorrhoidal masses. He tells you that he has had difficulty gaining weight in the past few years and admits to occasional heroin usage and multiple sexual partners. On examination, he appears emaciated with temporal wasting and lipodystrophy of the face. There are multiple moist, pink cauliflower-like 0.2 – 0.5 cm papules surrounding the anus. Digital rectal examination reveals gualac-negative, brown stool. He consents to whatever you think is appropriate management. At this time you should
(Note: Multiple partners, heroin usage, losing lots of weight seems like he is Immunocompromised)
A. Perform anoscopy
B. recommend increased fluid intake and a high fibre diet
C. refer him for resection of condylomata acuminata
D. refer him for resection of hemorrhoids
E. send studies for sexually transmitted diseases including HIV
Ans. E.
Question:
1.PV done in Virgin woman globally or not?
Answer: No, ACP recommends against performing screening pelvic examination in asymptomatic, nonpregnant, adult women (strong recommendation, moderate-quality evidence).
The current evidence shows that harms outweigh any demonstrated benefits associated with the screening pelvic examination. Indirect evidence showed that screening pelvic examination does not reduce mortality or morbidity rates in asymptomatic adult women, as 1 trial showed that screening for ovarian cancer with more sensitive tests (transvaginal ultrasonography and CA-125) also did not reduce mortality or morbidity rates. Because CA-125 and transvaginal ultrasonography found all cancer detected by the screening pelvic examination as well as additional cancer and this earlier detection did not lead to a reduction in morbidity or mortality rates, we conclude that the screening pelvic examination alone would also not reduce morbidity or mortality rates. No studies assessed the benefit of pelvic examination for other gynecologic conditions, such as asymptomatic pelvic inflammatory disease, benign conditions, or gynecologic cancer other than cervical or ovarian cancer. Also, there is low-quality evidence that screening pelvic examination leads to harms, including fear, anxiety, embarrassment, pain, and discomfort, and possibly prevents women from receiving medical care. In addition, false-positive screening results can lead to unnecessary laparoscopies or laparotomies. Note that this guideline is focused on screening asymptomatic women; full pelvic examination with bimanual examinations is indicated in some nonscreening clinical situations. This guideline does not address women who are due for cervical cancer screening. However, the recommended cervical cancer screening examination should be limited to visual inspection of the cervix and cervical swabs for cancer and human papillomavirus and should not entail a full pelvic examination.
2.Can Speculum Exam/ Pap smear be done for Virgin woman?
Yes, using a small Speculum, called as Paediatric Speculum.