Causes:
Nematodes (roundworms), trematodes (flukes), and cestodes (tapeworms).
1.Ascaris lumbricoides (Roundworms)
Infection may also be acquired through ingestion of contaminated fruits and vegetables. Most infected individuals are asymptomatic due to low worm load. Clinical manifestations occur due to pulmonary hypersensitivity and intestinal complications.
Symptoms:
Unexplained vomiting, abdominal pain, irritability, seeing worms in bathroom, pass worms in vomitus or feces.
Cx:
Poor growth and nutritional deficiencies in young child.
In heavy worm infestation, small bowel obstruction can occur due to a mass of entangled worms.
Worms migrate to aberrant sites such as biliary and pancreatic ducts, where they can cause cholecystitis, cholangitis, pancreatitis and rarely intra-hepatic abscess.
Inv:
Stool examination (ova and live parasites seen).
USG can identify worms in Pancreaticobiliary ducts.
Rx:
Albendazole 400mg OD (Taken with Food; fatty meal increases bioavailability) (DrugOfChoice-DOC)
Mebendazole 100mg q12h x 3d (or) 500mg OD. (DOC)
Ivermectin (BF) 150-200 ug/kg OD. (DOC)
Nitazoxanide Age 1-3y: 100mg Q12H x 3d (Optional)
Age 4-11y: 200mg Q12H x 3d
Age > 11y: 500mg Q12H x 3d.
2.Enterobius vermicularis (Pinworm or Threadworm)
Enterobius vermicularis is a small (1 cm long), white, threadlike worm that lives in the cecum, appendix, ileum and ascending colon. Eggs are not usually liberated in the gut. Gravid females migrate at night into the perianal region and release eggs there. The egg become infective within 6 hr. Perianal scratching causes transfer of eggs 10 finger nails. Infection occurs when eggs are ingested. The larvae hatch and mature within the intestine. Perianal itching, especially in night is the most common complaint.
Inv:
Stool microscopy is not useful as eggs are generally not passed in the stools. Eggs can be demonstrated by examining the perianal swab obtained early in the morning before the child has defecated.
Alternatively, a strip of transparent cellulose acetate tape is applied with sticky side down on the perianal region. The tape is lifted and pressed on a glass slide with the sticky side down.
Rx:
All the members of the family should be treated simultaneously to prevent cross-infection and reinfection. The nails of the child should be cut short and scrubbed. Single dose mebendazole or albendazole or pyrantel pamoate are highly effective. The course may be repeated after 2 weeks.
Dosage:
Albendazole (with food) 400mg OD. (DOC)
Mebendazole 100mg Q12H x 3d. (DOC)
Pyrantel Pamoate (suspension can be mixed with milk/fruit) 11mg/kg base (max 1g) OD; repeat in 2 weeks. (DOC)
3.Ancylostoma duodenale and Necator americanus (Hookworm):
Hookworm infestation is an important cause of iron deficiency anemia. Most infected persons are asymptomatic.
Symptoms:
Infective larvae may produce a pruritic maculopapular eruption known as ground itch; at the site of skin penetration.
Nonspecific complaints like abdominal pain, anorexia, and diarrhea have also been attributed to the hookworm infection.
Inv:
Still microscopy shows oval hookworm eggs.
Blood examination including Peripheral Smear which reveals microcytic, hypochromic anaemia, and total Eosinophil count as occasionally there is eosinophilia.
Rx:
For eradication of Worms:
Albendazole (with food) 400mg OD; repeat in 2 weeks. (DOC)
Mebendazole 100mg Q12H x 3d (or) 500mg OD. (DOC)
Pyrantel Pamoate (suspension) 11mg/kg base (max 1g) daily for 3days. (DOC)
For Anemia:
Oral Iron Therapy
Severe Anemia:
Packed Cell Transfusion
4.Filariasis:
Cause: Wuchereria bancrofti, Brugia Malawi or Brugia timori. These thread-like parasites reside in the lymphatic system of the host. Infestation is by Mosquito bites.
Epidemiology:
The infected mosquito bites a person and deposits the larvae in the skin. These may remain in the skin or cross this barrier to enter the lymphatics. In humans, larvae develop into adult male or female worms over a period of 4-6 months. Adult worms reside in afferent lymphatics. Adult female worms produce microfilariae that circulate in the bloodstream. The life cycle of the parasite is completed when a mosquito ingests microfilariae during a blood meal. Mosquito serves as the intermediate host in whom the microfilariae develop into infective larval stage
Symptoms:
Following the inoculation of infective larvae into man, a time lag of 8-16 months may occur before the clinical symptoms appear. Alternatively, microfilaremia may remain asymptomatic.
Clinical symptoms includes recurrent attacks of fever, lymphadenitis, lymphangitis.
Inv:
Peripheral Blood Smear demonstrates Microfilariae.
Examination of a thick blood film is still the best diagnostic tool. Adult worm may be detected in biopsy of lymph nodes. Lymphoscintigraphy may demonstrate lymphatic abnormalities even in asymptomatic patients.
Immuno Chromatographic Test (ICT) .
Serological: Patients with active filarial infection typically have elevated levels of antifilarial IgG4 in the blood and these can be detected using routine assays.
Rx:
Diethylcarbamazine is the drug of choice for lymphatic filariasis and is active against both adult worms and microfilariae. Repeated courses may be required for complete parasitic cure. Ivermectin is effective against microfilariae in a single oral dose of 400 µg/kg of body weight. A combination of ivermectin and albendazole is also effective in clearing microfilariae.
Dosage:
Diethlcarbamazine 2mg/kg Q8H x 12d (DOC)
Doxycycline 100-200mg OD x 6-8 weeks (Adjunctive; kills symbiotic bacteria within worms)
Albendazole (with food) 400mg OD (Adjunctive; reduces microfilaria)
Antihistamines or steroids (reduce allergic reactions to disintegrating microfilariae)
5.Tropical Pulmonary Eosinophilia:
Allergic and inflammatory response elicited by rapid clearance of micofilariae from bloodstream by immune mechanisms.
Symptoms: Paroxysmal nocturnal cough.
Dyspnea, fever, wheeze, loss of weight and easy fatiguability.
Lymphadenopathy and hepato-splenomegaly.
Rx:
Diethylcarbamazine 2mg/kg Q8H x 12-21d (DOC)
6.Visceral Larva Migrans:
Cause: Nematodes namely 1.Toxacara Canis (dog roundworm), 2.Toxocara cats (cat roundworm).
Symptoms: Fever, cough, wheezing, hepatomegaly, pulmonary, infiltration endophthalmitis and neurological disturbances.
Low grade fever with recurrent respiratory tract infections.
Marked eosinophilia is present.
Inv:
ELISA for Toxocaral antibodies.
Rx:
Albendazole and mebendazole are effective drugs. Alternative drugs include diethylcarbamazine and thiabendazole (25 mg/kg twice daily for 1-3 weeks).
Dosage:
Albendazole (with food) 400mg Q12H x 5d (upto 20d) (DOC)
Mebendazole 100-200mg Q12H x 5d (upto 20d) (DOC)
Corticosteroids (Adjunctive role in severe disease, eye involvement)
7.Cutaneous Larva Migrans:
Rx:
Albendazole (with food) 400mg OD x 3d (DOC)
Ivermectin (BF) 200 ug/kg OD x 1-2d
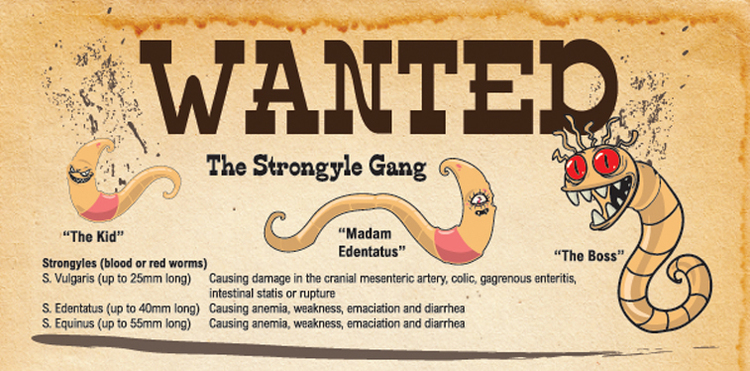
8.Strongyloidiasis:
Ivermectin (BF) 200 ug/kg OD x 2d (DOC)
Albendazole 400mg OD x 7d (Alternative)
9.Trichuriasis, whipworm:
Albendazole 400mg OD x 3d (DOC)
Mebendazole 100mg Q12H x 3d (Alternative)
Ivermectin (BF) 200ug/kg OD x 3d (Alternative)
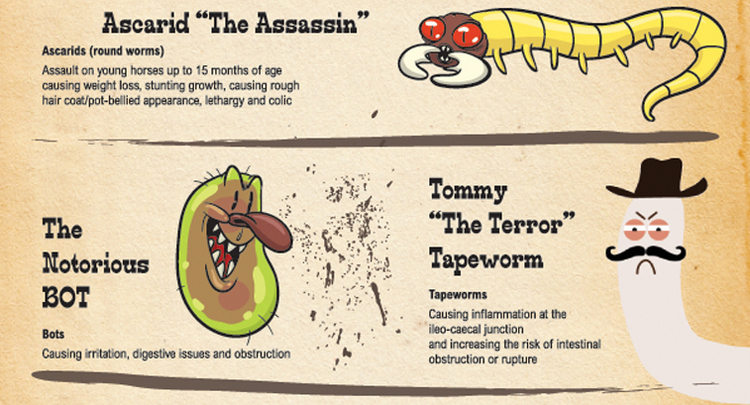
10.Taenia Solium and Saginata (Pork Tapeworm & Beef Tapeworm):
Symptoms:
Mostly Asymptomatic.
Non-specific complaints like nausea, pain in abdomen, and diarrhoea.
Cx: Carriers have an increased risk of developing cysticercosis by repeated auto infection, which may manifest as partial or generalised seizure, raised Intracranial tension, focal neurological deficits, or disturbances unconsciousness or behaviour.
Inv:
Patient may pass motile segments of worms through anus.
Stool exam shows eggs or proglottids.
For Neurocysticercosis: CT and MRI of brain.
Detection of Antibodies by enzyme-linked immunotransfer blot (EITB).
CSF eosinophilia.
Rx:
Adult Tapeworm:
Praziquantel (Taken with liquids during meal) 5-10mg/kg OD (DOC)
Niclosamide (Chewed or crushed and swallowed) 50mg/kg OD (Alternative)
Dwarf Tapeworm:
Praziquantel 25mg/kg OD (DOC)
Niclosamide weight5-15kg: 1g on day 1; then 500mg OD x 6d
>15kg: 1.5g on day 1; then 1g OD x 6d(Alternative).
11.Cysticercosis:
Albendazole 7.5mg/kg (max 400mg) Q12H x 8-30d (DOC)
Praziquantel 33.3mg/kg Q8H on day 1; then 16.7mg/kg Q8H x 29d (DOC)
Anticonvulsants (Adjunctive role in neurocysticercosis)
Corticosteroids; Surgery.
12.Echinococcosis:
Causes: E.granulosus or E.multilocularis.
Clinical: Hydatid disease or hydatidosis.
Symptoms: Liver cysts with abdominal pain and a palpable mass.
Lung cyst may present with chest pain, hemoptysis and breathlessness.
Passage of cyst in urine (hydatiduria).
Hematuria following hydatid disease of the kidneys.
Rupture or leakage from hydatid cyst may cause fever, itching, rash, anaphylaxis and dissemination of infectious scolices.
Inv:
Diagnosis is made by ultrasonography and CT scan. USG can reveal the internal membranes of cyst, floating ectogenic cyst material (hydatid sand) and daughter cysts within the parent cyst. These findings are of value in differentiating hydatid cyst from simple cysts of liver. Diagnostic aspiration is generally contraindicated because of risk of infection and anaphylaxis. Antibody detection by ELISA is more sensitive but less specific.
Rx:
When feasible, surgical removal of cyst is the definitive treatment.
Recently surgical excision has been replaced by USG or CT-guided percutaneous aspiration instillation of hypertonic saline or another scolicidal agent and aspiration after 15 min.
Medical Therapy:
Albendazole in a dose of 15 mg/kg/ day bid for two weeks repeated for 3-12 courses with 15 days drug-free interval in between two courses. The efficacy rate is 40-60%. The response to medical therapy is monitored by serial ultrasonography. Surgical removal can be contemplated for a large solitary cyst following albendazole therapy.
Dosage:
Albendazole 7.5mg/kg (max 400mg) Q12H x 1-6m (DOC)
Case Scenario:
Click to access 332f90bd84b0702c58d860e8f9916da474e9.pdf
Questions:
1.Intestinal infestation resistant to stat albendazole, what do you do?
Albendazole (with food) 400mg OD; repeat in 2 weeks. (DOC)
Mebendazole 100mg Q12H x 3d (or) 500mg OD. (DOC)
Pyrantel Pamoate (suspension) 11mg/kg base (max 1g) daily for 3days. (DOC)
2.Apart from Stool Examination, Hb, any other treatment/investigations need to be done?
Peripheral Smear, USG, Eosinophil count, ELISA.