^Common yet Imprecise symptom used to describe variety of common sensations.
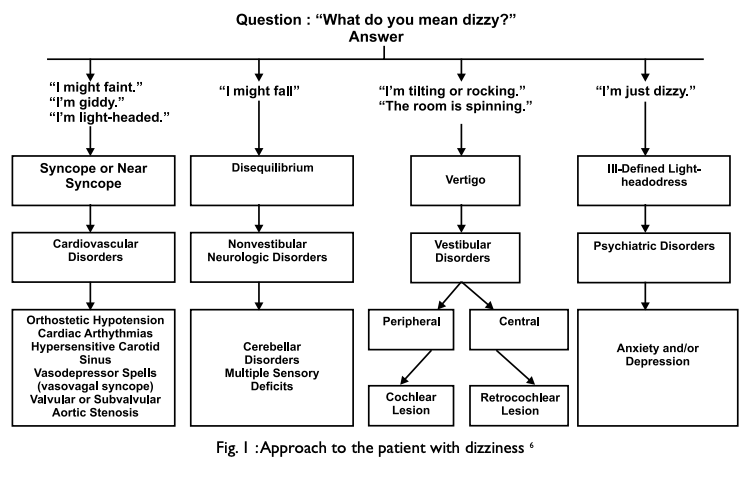
^It was traditionally divided into four categories based on the patient’s history: vertigo, presyncope, disequilibrium, and light-headedness.
^However, the distinction between these symptoms is of limited clinical usefulness. Patients have difficulty describing the quality of their symptoms but can more consistently identify the timing and triggers.
^The differential diagnosis is broad, the symptoms are vague, physicians must distinguish benign from serious causes that require urgent evaluation and treatment.
General Approach:
History Taking:
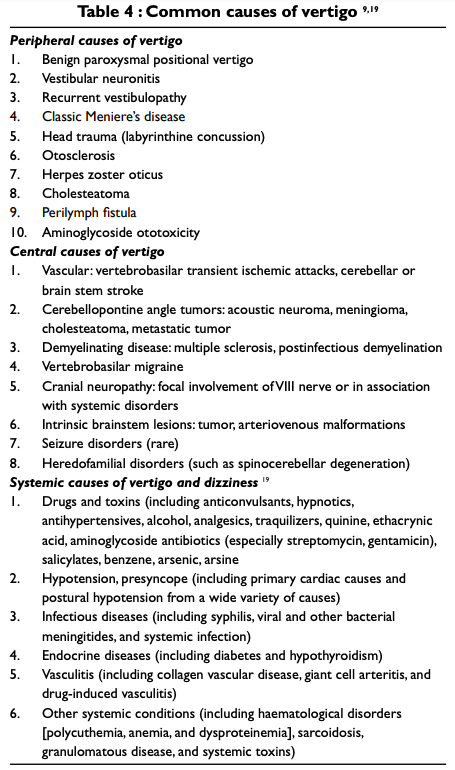
Dizziness can be divided into episodes that last for seconds, minutes, hours, or days. Common causes of brief dizziness (seconds) include benign paroxysmal positional vertigo (BPPV) and orthostatic hypotension, both of which typically are provoked by changes in head and body position. Attacks of vestibular migraine and Ménière’s disease can last hours. When episodes are of intermediate duration (minutes), transient ischemic attacks of the posterior circulation should be considered, although migraine and a number of other causes are also possible.
Symptoms that accompany vertigo may be helpful in distinguishing peripheral vestibular lesions from central causes. Unilateral hearing loss and other aural symptoms (ear pain, pressure, fullness) typically point to a peripheral cause. Because the auditory pathways quickly become bilateral upon entering the brainstem, central lesions are unlikely to cause unilateral hearing loss, unless the lesion lies near the root entry zone of the auditory nerve. Symptoms such as double vision, numbness, and limb ataxia suggest a brainstem or cerebellar lesion.

Examination:
- Complete Neurological Examination.
- Particular focus should be given to assessment of eye movements, vestibular function, and hearing.
- Audiometry should be performed whenever a vestibular disorder is suspected.
- Neuroimaging is important if a central vestibular disorder is suspected. In addition, patients with unexplained unilateral hearing loss or vestibular hypofunction should undergo magnetic resonance imaging (MRI) of the internal auditory canals, including administration of gadolinium, to rule out a schwannoma.
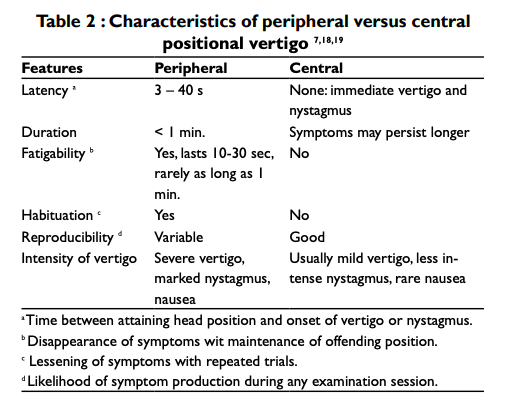
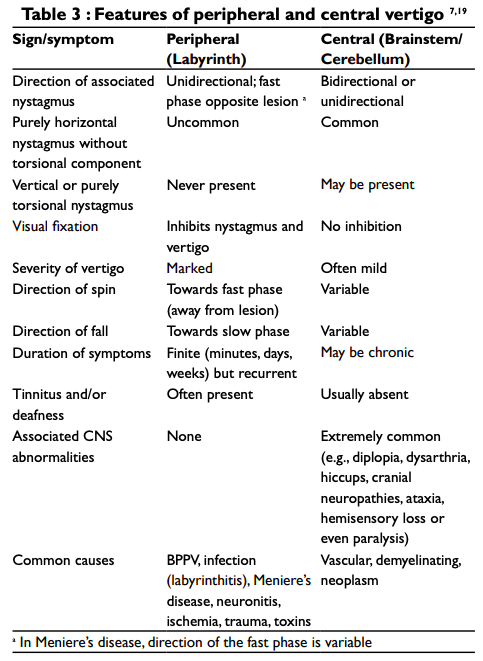
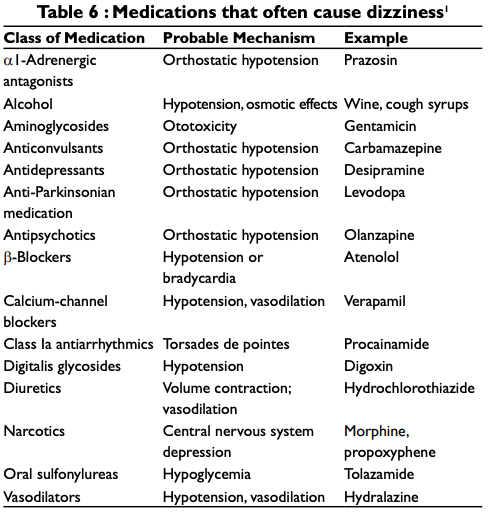
Causes & Differential Diagnosis:

Rx:
The treatment of dizziness or vertigo depends specifically on the cause. A detailed account of treatment modalities is out of the scope of this review. However, it should be born in mind that simply going on prescribing the vestibular suppressant drugs when the patient’s dizziness is due to orthostatic hypotension or due to some drug toxicity may not solve the purpose, rather may be detrimental. Thus, it is crucial to analyze the symptom of “dizziness” thoroughly to make the actual etiology clear before deciding the treatment modality.
Commonly used Medications for Suppression of Vertigo:
As noted, these medications should be reserved for short-term control of active vertigo, such as during the first few days of acute vestibular neuritis, or for acute attacks of Ménière’s disease. They are less helpful for chronic dizziness and, as previously stated, may hinder central compensation.
An exception is that benzodiazepines may attenuate psychosomatic dizziness and the associated anxiety, although SSRIs are generally preferable in such patients.
Vestibular rehabilitation therapy promotes central adaptation processes that compensate for vestibular loss and also may help habituate motion sensitivity and other symptoms of psychosomatic dizziness.
The general approach is to use a graded series of exercises that progressively challenge gaze stabilization and balance.
Dosage:
Antihistamines
- Meclizine 25-50mg TDS
- Dimenhydrinate 50mg OD/BD
- Promethazine 25mg BD/TDS (Can also be given rectally or IM)
Benzodiazepines:
- Diazepam 2.5mg OD/TDS
- Clonazepam 0.25mg OD/TDS
Anticholinergic
- Scopolamine transdermal (Patch)
Physical Therapy:
- Repositioning manoeuvres
- Vestibular Rehabilitation

