Causes of Obesity:
1.Eating too much and moving too little
Physically active man needs 2.5k calories a day,
Physically active woman needs 2k calories a day.
2.Poor diet
^Eating large amount of processed or fast food (high in fat & sugar)
^drinking too much alcohol (contains lot of calories)
^eating out a lot (temptation + food can be higher in fat & sugar)
^eating larger portions than you need
^drinking too many sugary drinks (soft drinks, fruit juice)
^comfort eating (low self-esteem, depression)
3.Lack of physical activity
The Department of Health and Social Care recommends that adults do at least 150 minutes of moderate-intensity aerobic activity, such as cycling or fast walking, every week. This does not need to be done all in a single session, but can be broken down into smaller periods. For example, you could exercise for 30 minutes a day for 5 days a week.
4.Genetics (very rare)
Prader-Willi Syndrome (fault in Chromosome 15)
5.Medical reasons
^Underactive thyroid gland (Hypothyroidism)
^Cushing’s syndrome (overproduction of steroid hormones)
6.Certain Medicines can contribute to weight gain
^Corticosteroids
^Medications for epilepsy and diabetes (Sodium valproate and Sulphonylureas)
^certain antidepressants (Tricyclic antidepressants)
^medicines for Schizophrenia
^Beta-blockers
^Oestrogen-containing contraceptive pill
^weight gain can sometimes be a side effect of stopping smoking.
Cx:
^Quality of life
^Sleep apnea
^Infertility
^Gout
^High blood pressure
^Diabetes
^Cancer
^Coronary Heart Disease
^Gall Stones
^Arthritis
Dx:
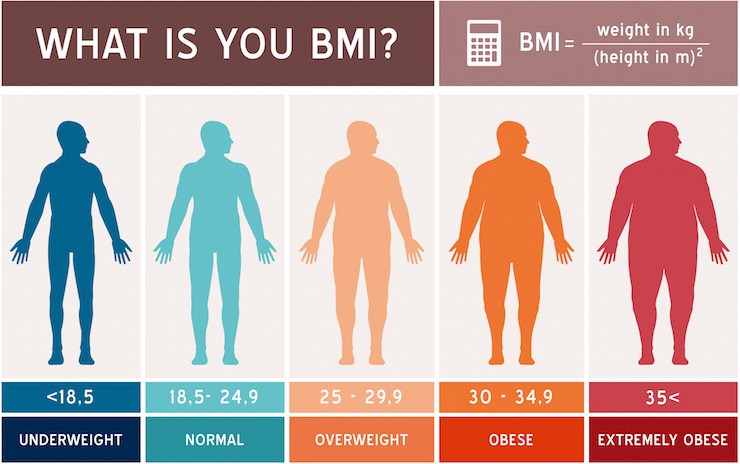
^BMI (>30) (Wt in kg/ht in m)
^History taking (lifestyle, underlying cause, mental health, family h/o)
^Blood pressure (HTN risk)
^Blood sugar (DM risk)
^Lipid profile
^Waist circumference (People with very large waists, generally, 94cm or more in men and 80cm or more in women develop obesity related health problems)
Rx:
^Healthy balanced diet
^Physical activity
^Diet – There’s no single rule that applies to everyone, but to lose weight at a safe and sustainable rate of 0.5 to 1kg a week, most people are advised to reduce their energy intake by 600 calories a day. Try to avoid foods containing high levels of salt because they can raise your blood pressure, which can be dangerous for people who are already obese.
^Supervised low-calorie diet
^Avoiding weight regain: It’s important to remember that as you lose weight your body needs less food (calories), so after a few months, weight loss slows and levels off, even if you continue to follow a diet. If you go back to your previous calorie intake once you’ve lost weight, it’s very likely you’ll put the weight back on. Increasing physical activity to up to 60 minutes a day and continuing to watch what you eat may help you keep the weight off.
Medication:
1.Orlistat (Pancreatic lipase inhibitor)
Dose: 120mg TDS (fat absorption inhibited by 30%) (effective in patient suffering from type 2 dm)
2.Sibutramine (Serotonin-norepinephrine reuptake inhibitor)
Dose: 5-15mg/day (Inhibits reuptake of Serotonin; norepinephrine at hypothalamic sties).
Note: Withdrawn in certain countries due to increased Cardiovascular risks.
3.Rimonobant (Cannabinoid type-1 receptor antagonist)
(Developed for smoking cessation; facilitate weight loss)
Note: Withdrawn in certain countries due to serious psychiatric side effects.
4.Lorcaserin (Serotonin 2C receptor agonist -> Promotes satiety) (Adjunct to low calorie diet and ^physical activity)
Dose: 10mg BD
5.Phentermine & Topiramate (Qsymia)
Mediates release of catecholamine’s; reduced appetite; decreased food consumption.
Dose: 3.7mg/23mg OD x 14 days & then;
Increase to 7.5mg/46mg OD.
After 12 weeks, <3% weight loss -> discontinue.
High Dose: 15mg/90mg (PHEN/TPM) OD.
6.Naltrexone & Bupropion (Contrave)
MOA: Combined to dampen the motivation that food brings (dopamine effect) and the pleasure of eating (opioid effect).
Dose: 32mg/360mg (Naltrexone-Bupropion)
7.Liraglutide
MOA: Weight loss effects via hypothalamic neural activation causing appetite suppression.
Dose: 3mg OD, injected s/c.
Surgery:
1.Bariatric Surgery (Laproscopically)
Goal: Disrupting release of ghrelin (the hormone responsible for increasing food intake by increasing size and number of meals) and other peptides -> enhancing satiety.
Efficacy of Orlistat:
Context:
Rapidly rising prevalence of obesity is alarming. Obesity predisposes to co-morbidities like hypertension, type 2 diabetes mellitus, dyslipidemias, thus substantially rising healthcare expenditure. Lifestyle modifications alone have very limited success, necessitating the addition of pharmacotherapy to it.
Objective:
Present study was carried out to evaluate the efficacy and safety of orlistat in obese patients.
Materials and Methods:
Eighty obese (BMI>30) patients according to inclusion and exclusion criteria were randomized into either of the two groups. Group 1 received orlistat 120 mg three times a day and group 2 received placebo three times a day. Weight, waist circumference, BMI, total cholesterol, triglycerides, HDL, LDL were measured at baseline and then at 8th, 16th and 24th week. ADR reported by patients were recorded. For safety evaluation various hematological and biochemical parameters were assessed. Z test was used for analysis of data.
Results:
Compared to placebo, orlistat caused significant reduction (P<0.05) in weight (4.65 kg vs 2.5 kg; orlistat vs placebo, respectively), BMI (1.91 kg/m2 vs 0.64 kg/m2) and waist circumference (4.84 cm vs 2 cm), cholesterol (10.68 mg vs 6.18 mg) and LDL level (5.87 mg vs 2.33 mg). In the orlistat group, the GI side effects like loose stools, oily stools/spotting, abdominal pain and fecal urgency were observed.
Conclusion:
Orlistat is an effective and well-tolerated antiobesity drug, which can be employed as an adjunct to therapeutic lifestyle changes to achieve and maintain optimal weight.
Source:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3125014
Anti-Obesity Drugs (Safety and Efficacy):